Neuromodulation Information
Where Personalised Pain Relief Matters!
1. Introduction
At Pain Relief Ireland, we are dedicated to ensuring that we personalise your pain relief. The use of neuromodulation devices can deliver life-changing therapies to chronic pain patients.
We specialise in offering individuals the best in neuromodulation technology to treat chronic pain and we have experience in an array of devices which will ensure you receive the best device to personalise your therapy.
Education is an important part of this process and we want to provide you with the information to help you understand what neuromodulation is, how the technology can be used to relieve your pain and how it can improve your quality of life.
Pain is specific to each individual. It is therefore important that you use this information in conjunction with your pain consultant so that together you will be able to come to a decision that offers the best outcome for you in the long-term.
Are you a candidate for Neuromodulation?
Click the Neuromodulation Survey button below and answer the following questions to find out.
Neuromodulation Survey
Download Information Booklet (PDF)
Neuromodulation is when a device that provides electronic current is used to change / control some of the pain messages that your body sends to your brain. This can be in the form of a traditional spinal cord stimulator, which is implanted near the spinal cord, or it may be a more focused device that targets a specific nerve or nerves. Neuromodulation offers personalised pain relief.
When neuromodulation works well there are several advantages such as:
- It can dramatically change the pain intensity you feel so that you are placed in
control of your life again. - It offers you the ability to use specific programs/settings that match your daily requirements which you can change as you need.
- It offers you the opportunity to increase your activity levels including walking, swimming, gym and even returning to some forms of employment
- It helps in reducing and often eliminating the long-term need for oral medication
- Neuromodulation can offer you the opportunity to start to do more with your life.
2.1. What type of device is used?
There are different makes and models of devices available. Your consultant will propose a specific make / model that will match your requirements best. Irrespective of the model of the device there are some common principles involved in all models.
2.2. What are the “settings” used on the device?
All devices will be programmed with specific parameters matched specifically for your pain intensity and pain pattern. For some individuals, low frequency stimulation, where you feel some tingling (paraesthesia) will be used. For other patients higher frequency stimulation, where you cannot feel anything, will be the best treatment for the pain.
- It is often necessary to try a few different combinations to establish which setting is most comfortable for you and the one which provides you with the best relief.
- It is not uncommon that these settings may need to be modified as your activity levels increase.
- It is important that you get these settings reviewed regularly to ensure you gain the most benefit from your device.
3.1. Indications
A spinal cord stimulator can only treat certain types of pain. The National Institute for Health and Care Excellence (NICE) is the organisation responsible for recommending which treatments are useful. NICE recommends spinal cord stimulation for the following diagnosed conditions:
- Neuropathic pain. This refers to pain which is caused by an insult or injury to the nerves, rather than pain caused by damage to the other tissues, such as the joints and muscles.
- Failed back surgery syndrome, when patients are suffering with neuropathic pain, rather than mechanical pain. This is persistent pain despite having surgery on the lower back. There is evidence that persistent pain after neck surgery can also benefit from this treatment.
- Complex regional pain syndrome (CRPS).
- Post Laminectomy pain, disc surgery and degenerative disc disease and adhesions in the epidural space ( i.e. arachnoiditis or lumbar adhesive arachnoiditis) can benefit.
- Spinal cord stimulation is recommended for patients who have severe chronic pain that is limiting their daily life and who have already tried all reasonable, more traditional therapies such as painkillers and physiotherapy.
- Peripheral neuromodulation usually targets a specific nerve or group of nerves to control the pain pathway.
3.2. What can a spinal cord stimulator achieve?
A spinal cord stimulator cannot be used as a standalone treatment for chronic pain. At Pain Relief Ireland, in keeping with international recommendations, we ensure that all individuals who are being considered for a spinal cord stimulator are assessed by a multidisciplinary team. This may include specialist doctors/surgeons, clinical nurse specialists, physiotherapists, occupational therapists, industry technical support and psychologists as required. The treatment pathway (or treatment plan) follows this guidance, and in order to ensure the best possible care, patients must engage with some or all elements of the treatment pathway.
Just as pain is unique to each individual, each individual will have a unique treatment plan designed to meet these needs. A spinal cord stimulator is an important instrument in achieving this goal. At Pain Relief Ireland we believe that the most important criteria that must be present before a spinal cord stimulator can be considered is the willingness of the individual to embrace change. A device can o!er each individual a fantastic opportunity to improve one’s quality of life but it requires work. Pain relief Ireland is prepared to support you in every way possible to achieve your goals.
3.3. How effective are spinal cord stimulators?
Spinal-cord stimulators help some people more than others. In general a target of 50-70% reduction in pain intensity and pain medication is set. Improvement in an individual’s ability to move or sleep is also expected. At Pain Relief Ireland we believe that individuals who have the willingness to embrace
change find neuromodulation most effective. Ask your specialist what the results are for people with your particular condition.
4.1. How does a spinal cord stimulator work?
The concept of using electricity to treat pain has been used for many centuries. Researchers have struggled to understand precisely why small amounts of an electronic current, focused on specific parts of the spinal cord or at a nerve fiber, can change the way in which pain signals are processed. What is known is that the presence of a small dose of electrical current “modulates” the feeling of “pain” and replaces it with a non-painful signal in the area of your body that normally hurts. If the spinal-cord stimulator is successful, you will find that the “pain sensation” is replaced by another more pleasant sensation. In some cases technical
settings can be used to deliver pain relief with no “sensation”. Each individual will have a unique treatment plan designed to meet these needs. A spinal cord stimulator is an important instrument in achieving this goal.
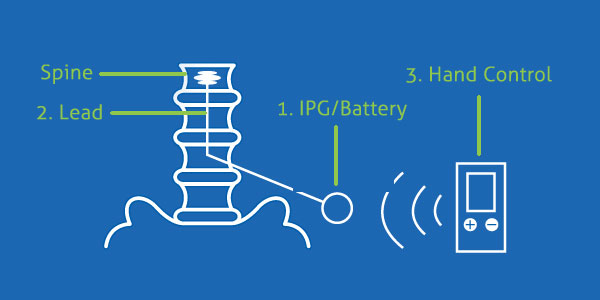
4.2. Components of a spinal cord stimulator
Whatever type of spinal-cord stimulator you have, there a number of key aspects in the treatment plan. There are usually three parts to a spinal-cord stimulator.
- The Implanted Power Generated (IPG) or “The Battery”. This is the very small computer that controls the stimulating system. This is usually located under the skin in your buttock region, or other suitable area. The computer has its own battery and generally they are rechargeable devices. Secure wireless programming and electronic transfer of data is possible.
- A electronic lead / electrode. Each lead has a set of electrodes where the electric current is transferred to the target tissue. The position of the “lead” is crucial to the optimization of your device. The lead allows tiny amounts of electrical current reach your spinal cord. This is very accurate and safe.
- A hand-held controller. You can use this to switch the spinal-cord stimulator on or off and to adjust it until you feel a pleasant tingling in the area where you normally feel pain. You can carry the controller around with you - it’s about the same size as a mobile phone. This is a bluetooth communication tool that gives you the flexibility to control your pain therapy.
4.3. What are the risks of having a spinal cord stimulator?
There are some risks associated with any operation. Most of the common issues that arise with spinal cord stimulators are minor, but there are a few rare problems that you should know about. It is important that you ask your specialists about how common the following problems are.
| Table 1 Key Issues | Incidence |
| Wound / Scar discomfort
| Common >50% |
| Post-operative wound infection
| 5% (1 in 20 cases) <1% |
| Lead Migration
| 5-10% cases in first 8 weeks then <2% |
| Headache
| 10% |
| Nerve Injury
| <1% |
| Other Issues |
|
|
|
|
|
|
4.4. Typical Patient Pathway
When you’ve had your operation, there are a few extra things that you should know about.
Clinical Assessment
Neuromodulation recommended by Pain Consultant
Pre-Certification Process
Psychology Assessment
Education & Technology Session
(see section 7.1)
QST / Pre-op Admission
Introduction to Get Ready Monitoring (see section 7.2)
Implantation Stage
Option A: Trial Stage
7 Day trial followed by clinical review
Option B: Full Implant Stage
24 hours overnight admission
Follow up plan
Programming session at week 2, week 6 and week 12 will be arranged
(see section 4.5)
4.5. Follow up and aftercare
Once you have had your device implanted a number of things will happen. While we personalised the care plan on a case-by-case basis in general you can expect:
- To be discharged home within 24 hours of surgery.
- An initial stimulation program will be put in place but occasionally we may defer until you are comfortable.
- At the 14 day follow up clinic a detailed programming plan will be arranged, and targets set.
- You may be offered access to our “Get Ready” platform to monitor your progress remotely.
- Any issues with wounds or post operative recovery can be addressed either via the GP or in the clinic.
- Depending on the level and progress of the programming plan we may ask you to attend a second programming clinic to improve the situation based on your experience.
- We would encourage a graded return to exercise.
- Review with Prof. Hegarty at approximately 3 months to assess and plan ahead.
For the trial or “on-table” trial to be considered a success the device must be able to cover 80% of your painful area. Your consultant will explain which approach is best for you.
- If you have a 7-day trial then it should be possible to see a significant impact on your quality of life and on the intensity of your pain even in this time. We expect it to reduce your pain by >60% and improve your sleep pattern. There is often a decrease in the daily analgesic requirement to deal with breakthrough pain during a trial.
- You will be asked to keep a pain diary for the duration of the trial and this will be examined with you at the end of the 7 day trial.
- If the trial results in a moderate impact, it is not considered successful. This is because the amount of pain relief provided by the spinal cord stimulator will reduce over time.
- If your pain does not respond to spinal cord stimulation we shall consider a review of all the other options to support individuals going forward. It is far better to avoid the inappropriate surgical implant of a spinal cord stimulator than to simply put it in because it “seems like a good idea”.
We seek to personalise the longterm plan when the stimulators are in place. Our centre has been at the forefront of research and clinical practice development over the years and continue to identify way to optimise outcomes for indivduals bases on your preferences. We will work with you to achieve this.
7.1. Educational Session
Spinal cord stimulation is the most advance technology available to help chronic pain management. There are several products each with unique features. We understand that not everyone is comfortable with technology, so we aim to simplify it as much possible.
Our clinical nursing team will with work with you to give you the best information in a simple way. We do not want you to be afraid of the technology but instead we want you to get the most you can from it.
It is our experience that individuals who engage with this step find it very helpful. We also find that having a second person attend with you who can help improves the outcome.
These sessions are also a good opportunity to ask questions about the device and outcome targets. We occasionally run patient educational days to help refresh and update individuals. Contact detail on dates, course content and how to reserve a space.
7.2. Get Ready
The “Get Ready TM” platform is a unique digital management system Pain Relief Ireland has adapted to allow us help you achieve your goals. The system has been designed not to be intrusive but to give you greater access to management. It meets all the compliance, data and privacy requirements.
The system in an app-based program that you can interact with and that your pain team can review. It provides you with a user-friendly option to ensure we can help in the best way possible.
You do not have to use this system but most individuals find it very useful. Our nursing team will introduce you to the platform and help organise your log in details.
We are committed to handle all Personal Data with the following values in mind:
- Compliance with legislation: facilitating your own compliance for your health services;
- State of the art: always using up to date technical standards;
- Privacy by design and by default; privacy is built-in and activated from the start;
- Transparency and control; for you and only using trustworthy third parties;
- Security measures; using the industry standard information security mechanisms to protect sensitive health data.
We hope this information will help answer your questions and we will be happy to address any other issues with you.
The introduction of neuromodulation as a treatment option is an important decision that needs to be made by comparing all other possible options. This will increase the chance of long-term success.
At Pain Relief Ireland we believe that the willingness of the individual to embrace change is the most important criteria that must be present before neuromodulation is considered.
Neuromodulation can offer an individual a fantastic opportunity to improve their quality of life but it requires work and effort. Pain Relief Ireland is prepared to support you in every way possible to achieve your goals.
Disclaimer: This information is to assist individuals understand the key goals of neuromodulation and it should not replace the opinion of the pain consultant.
Patient Success Story
Laura, a nurse, wife, and mother of 3, was diagnosed with bowel cancer in 2017 at age 38. She made a great recovery following major surgery—except for lingering pain in her hip and back.
“I tried everything to help myself.” However, acupuncture, physiotherapy, prescription medications, and injections didn’t give her any lasting relief. Her daily pain level averaged 7-8, and she soon needed a crutch to walk.
“It was so frustrating,” said Laura. “I felt from day one after the surgery that this was nerve pain, but no one heard or listened to me.” She started doing research and found a specialist who offered Nevro HFX. “I was prepared to go anywhere in the world to try this.”
In June 2021, Laura met with Prof Dominic Hegarty at Pain Relief Ireland, who determined she was a good candidate for HFX. That September, she received the implant. After working with her Nevro HFX Care Team to find the right settings, Laura found significant relief: no leg pain and minimal hip and low back pain.
"I can honestly say HFX has changed my life..."
Nearly 2 years later, her pain level averages 2-4 now. “I can honestly say HFX has changed my life. I am back to work 2 days a week, walking 5 km, and cycling with my family. These are activities that I never thought I’d ever be able to do again.”
Results may vary. *HFX is a comprehensive solution that includes a Senza spinal cord stimulation system and support services for the treatment of chronic pain.


Contact Us
Contact us and let us help you to take control of your pain.
If you would like us to set up an appointment please contact us on 021-235 5500 or email info@painreliefireland.ie
If you require a first time appointment ask your GP to forward a referral and we shall contact you.







